Diagnosis
Without a diagnosis individuals with FASD are being incorrectly labeled and judged every day. A diagnosis gives a person a better understanding of themselves, and those around them a lens to see symptoms versus behaviours.
Early diagnosis of Fetal Alcohol Spectrum Disorder (FASD) is important for creating an understanding of an individual’s strengths and challenges. Appropriate early intervention and support services can mitigate the development of executive functioning and daily living challenges associated with this hidden neurodevelopmental disability, and promote healthier outcomes.
Everyone has a story…
People with Fetal Alcohol Spectrum Disorder (FASD) all vary in how they present the disorder. Each person is different depending on timing, frequency, and the amount of alcohol the fetus was exposed to during pregnancy. We also know that Adverse Childhood Experiences (ACEs) affect a child’s development. Arguably, a child with FASD has experienced ACEs since conception, not just since birth. They will all present different symptoms.
Their story is a critical piece of the assessment and diagnostic puzzle for individuals with FASD.
FASD is a diagnosis of elimination. According to The Canadian Medical Association, it takes a skilled, multi-disciplinary team including a physician, psychologist, Speech-Language Pathologist (SLP) and an Occupational Therapist to diagnose FASD. Caregivers and support professionals are often asked to complete documentation to provide data for the diagnosis.
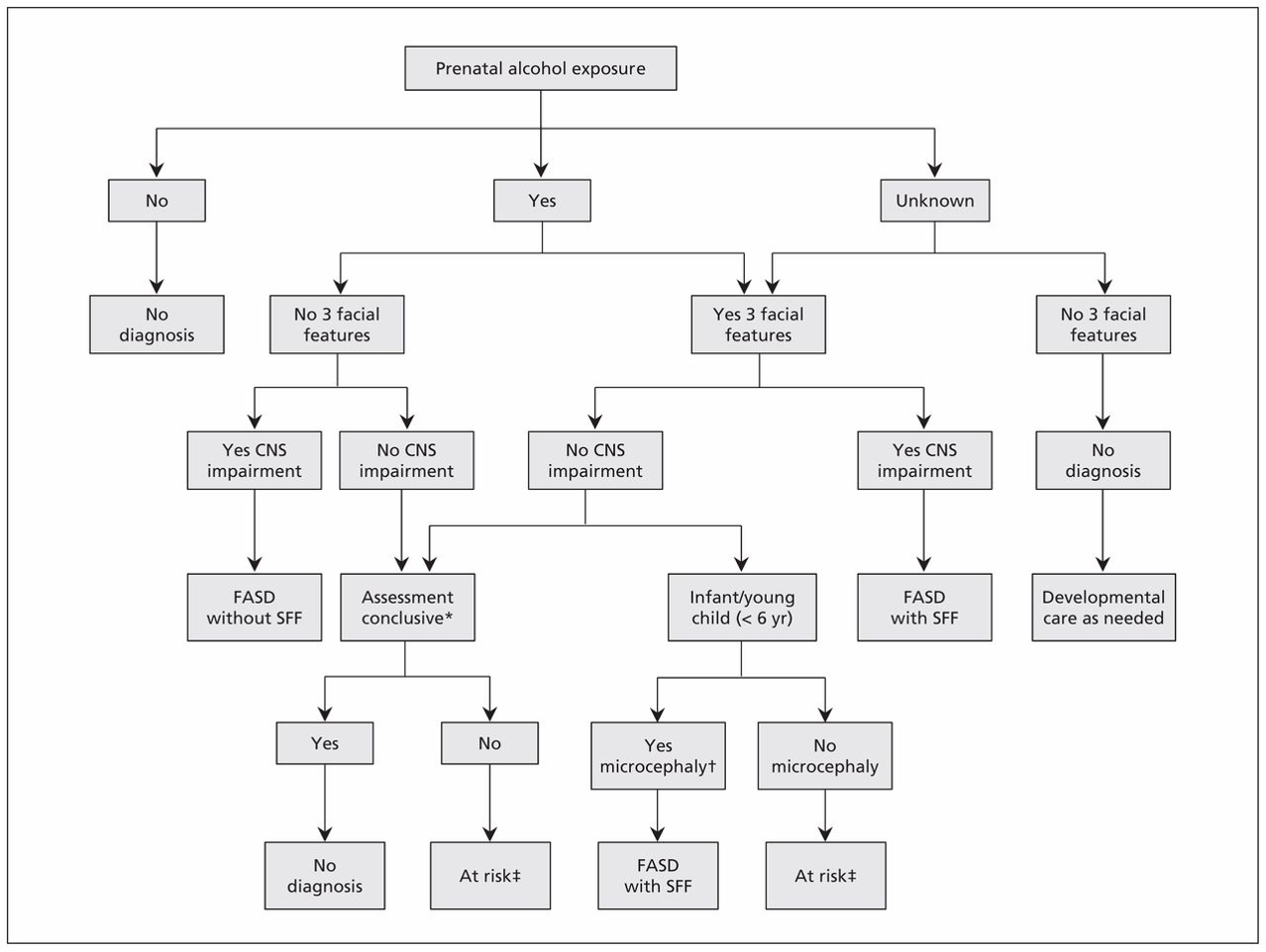
The Current Canadian Medical Association Guidelines for FASD Diagnosis
CMAJ, Vol. 188, Issue 3, 16 Feb 2016
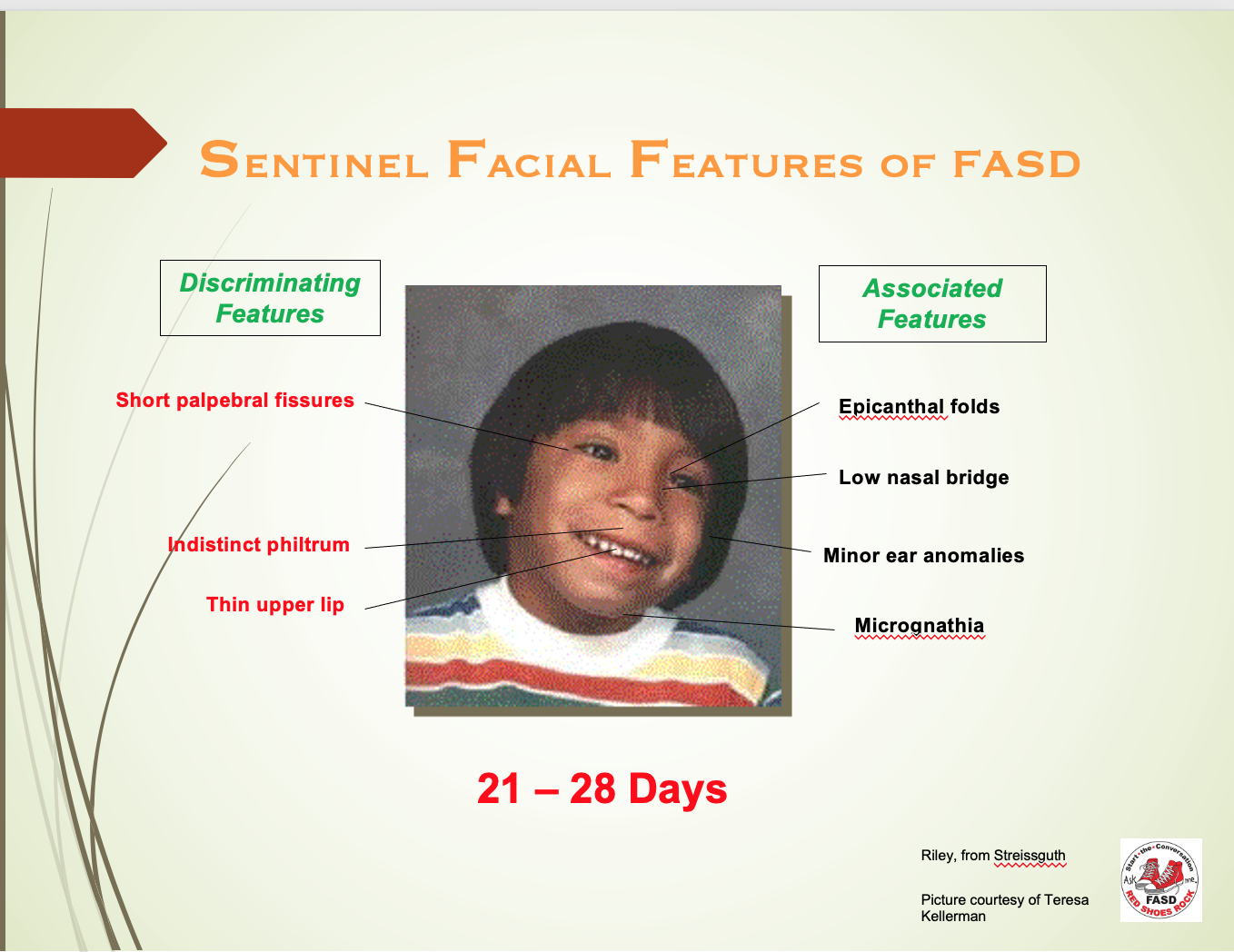
Short Palpebral Fissures, an indistinct philtrum and a thin upper lip are the medical triad of facial features associated with FASD. These features develop between the 21st and 28th of pregnancy. However, if no alcohol is consumed during this period, the facial features will not be evident.
Because 90% of those affected by Prenatal Exposure to Alcohol do not have the sentinel facial features, we often have normal expectations from them, which is the source of frustration and therefore, reactive behaviour, better described as symptoms of FASD.
So…
Specifically challenging are individuals diagnosed with FASD without Sentinel Facial Features.
They do not have the facial features but show challenges in at least three brain domains. They look normal but have trouble negotiating “life”.
A lived experience…
Where do I get a diagnosis for FASD in Nova Scotia?
Balance Psychology - Dual Province FASD Clinic
Full service, a multi-disciplinary diagnostic clinic providing assessments by a Paediatrician/Physician, Psychologist, Occupational Therapist (O/T), and Speech Language Pathologist (SLP). They provide clinical follow-up with families, schools, courts etc.
Dr. Robert McInerney, Ph.D, R. Psych
Dr. McInerney is a neuropsychologist in Halifax, Nova Scotia. Over the past 23 years, he has worked in several major hospitals and community settings in British Columbia, Alberta, Ontario, and Nova Scotia. He is a Clinical Associate at Dalhousie University and a former member of the executive committee of the Association of Psychologists of Nova Scotia (APNS).
IWK Health FASD Clinic
The IWK Complex Care Clinic completes diagnoses, including a multi-disciplinary FASD diagnostic service for children. A referral from your doctor is required.
Wije’winen Health Clinic
Wije’winen Health Clinic is a program of the Mi’kmaw Native Friendship Centre. The Health Clinic partners with Balance Psychology to provide a culturally sensitive, full-service, multi-disciplinary diagnostic experience.
Learn more about FASD Diagnosis by exploring additional resources.
Dive Deeper
References
https://www.cmaj.ca/content/suppl/2015/12/14/cmaj.141593.DC1 Cook, JL, Green CR, Lilley CM, et al.; Canada Fetal Alcohol Spectrum Disorder Research Network. Fetal Alcohol Spectrum Disorder (FASD); a guideline for diagnosis across the lifespan. CMAJ 2015. DOI:10.1503/cmaj.141593.
https://canfasd.ca/wp-content/uploads/publications/FASD-Clinic-Process.pdfhttps://doi.org/10.1503/cmaj.14159
Government of the United States (2024, May 16). Adverse Childhood Experiences. CDC (Center for Disease Control). Retrieved July 12, 2024, from https://www.cdc.gov/aces/about/index.html